Search for a POS Provider
If you have a POS plan, you have access to a variety of benefits and covered services with a 3-tier design. Each tier mixes flexibility and costs. You control your out-of-pocket expenses while receiving a full range of health care benefits. You may choose to access care from any tier - every time you seek health care.
Tier I benefits (HMO)
Tier I benefits give you the most value for the least out-of-pockets costs. Most services have set copayments with no calendar year deductible or coinsurance. Your HPN primary care provider will arrange for most of the covered services available under this benefit tier. Low copayments make quality health care affordable.
Tier I providers are included in the Health Plan of Nevada HMO provider directory:
- Southern Nevada (Clark and Nye counties in Nevada and Mohave County in Arizona)
- Northern/Rural Nevada (all other Nevada counties)
Tier II Benefits (Expanded Plan Provider)
Tier II benefits give you additional provider choices with set copayments for routine care. After meeting a calendar year deductible, you will pay coinsurance for non-routine covered services.
Tier II Expanded Plan providers are included in the provider directories for Sierra Health and Life, Northern Nevada Health Network and UnitedHealthcare Choice Plus.
- Southern Nevada (Clark and Nye counties in Nevada and Mohave County in Arizona)
- Northern/Rural Nevada (all other Nevada counties)
- Utah
Outside of Nevada, Mohave County, AZ, or Washington County, UT
You may have access to the Choice Plus network of providers outside of the state of Nevada and Mohave County, Arizona and Washington County, Utah.
Please note: UnitedHealthcare Choice Plus Network must appear on the back of your health plan ID card in the area labeled Network in order to access the Choice Plus network. (See red highlighted area below.)
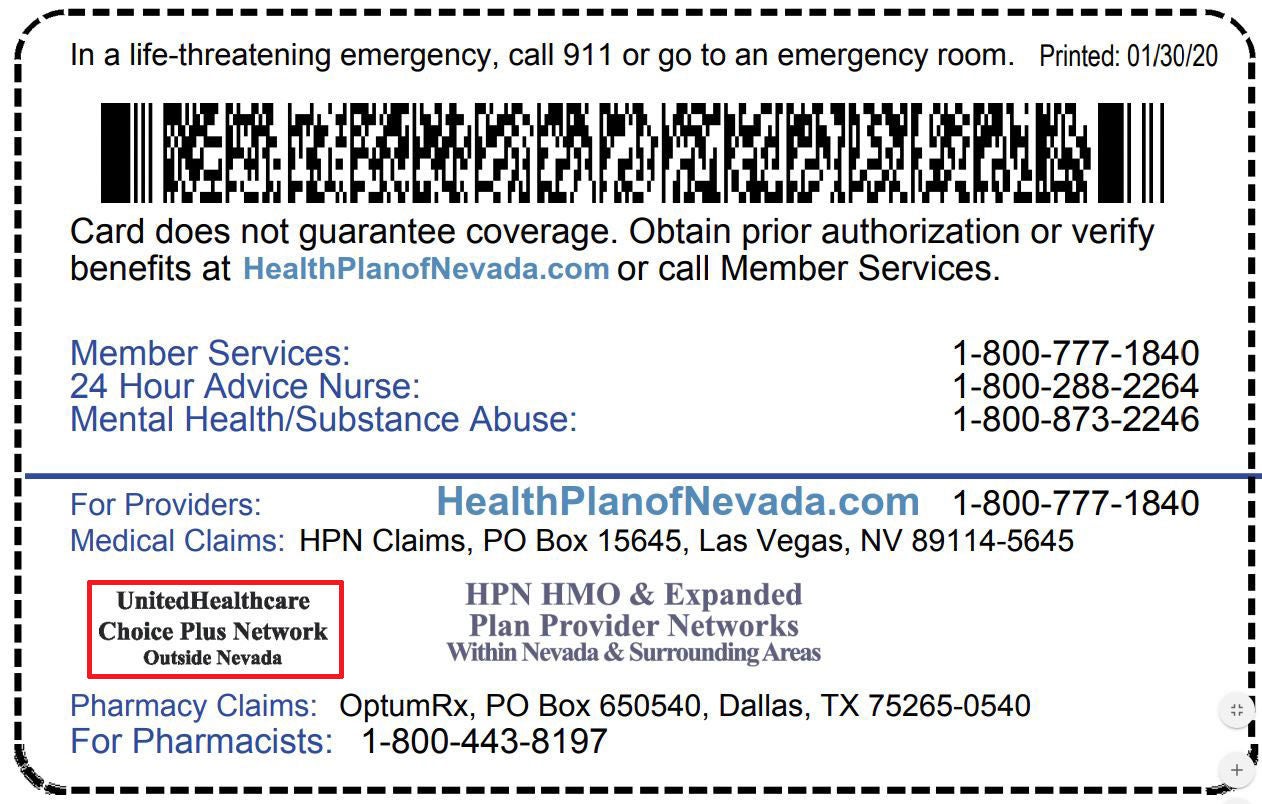
If your card includes the UnitedHealthcare Choice Plus network, use the All Other Service Areas Provider search.
Tier III Benefits (Non-Plan Provider)
Tier III benefits give you the choice to see any licensed health care provider. This benefit level offers you the most provider options, but your out-of-pocket costs will be higher. All non-emergency services have a calendar year deductible and a higher coinsurance payment than under the tier II benefit level. Please note that Tier III Non-Plan Providers do not accept the HPN Reimbursement Schedule as payment in full for covered services. This means you will be responsible for any fees charged by the Non-Plan Provider that exceed the HPN Reimbursement Schedule.
Tier III includes any licensed health care provider.
Members please note that although certain facilities are listed as plan providers, the professional services for interpretations or certain diagnostics (to include, but not limited to, cardiology, emergency medicine, neurology, and pulmonology services) may be rendered by non-plan providers. The patient may be responsible for services rendered by non-plan providers.